Healthcare in the U.S. is in crisis. Compared to other nations with large economies, America spends the most money on healthcare by far yet has significantly worse patient outcomes.
One of the most promising approaches to addressing this crisis is value-based care (VBC), which is based on a simple but profound concept: pay for improved outcomes not for volume of services. VBC radically changes the incentives for healthcare providers. Instead of being rewarded for doing more, they’re rewarded for achieving more.
Currently, most healthcare in the U.S. is delivered via “fee-for-service” arrangements. Providers are paid for each service: an office visit, a CAT scan, surgery, etc. Under VBC, providers are compensated based on the outcome of care provided: have patient conditions improved, and is the delivery of care more efficient?
The promise of VBC is driving adoption of the model and the numerous information-sharing standards that support it . Leading the effort has been the Centers for Medicare & Medicaid Services (CMS), which has set a goal to have 100 percent of Medicare beneficiaries and most Medicaid beneficiaries in accountable care relationships by 2030. In addition, many large healthcare entities – including HMOs, insurers, and large practices of primary care providers – have adopted policies in support of VBC goals.
The Challenge of Data Complexity in the VBC Model
The success of VBC depends on the availability, quality, and usability of massive amounts of data. The right information must reach the right people (patients, providers, payers) at the right time. Any delays in storing, normalizing, and analyzing data can threaten the quality of patient care by postponing accurate diagnosis, treatment, and/or follow-up.
Just as important is patient-outcome data specifically for VBC, which practitioners can use to benchmark and identify best practices. One of the key gating factors to increased VBC adoption is access to data about treatment outcomes. The healthcare ecosystem needs integrated data records that adhere to available standards. The holy grail would be a single longitudinal record containing all patient information that can be shared seamlessly among all involved parties in the healthcare ecosystem.
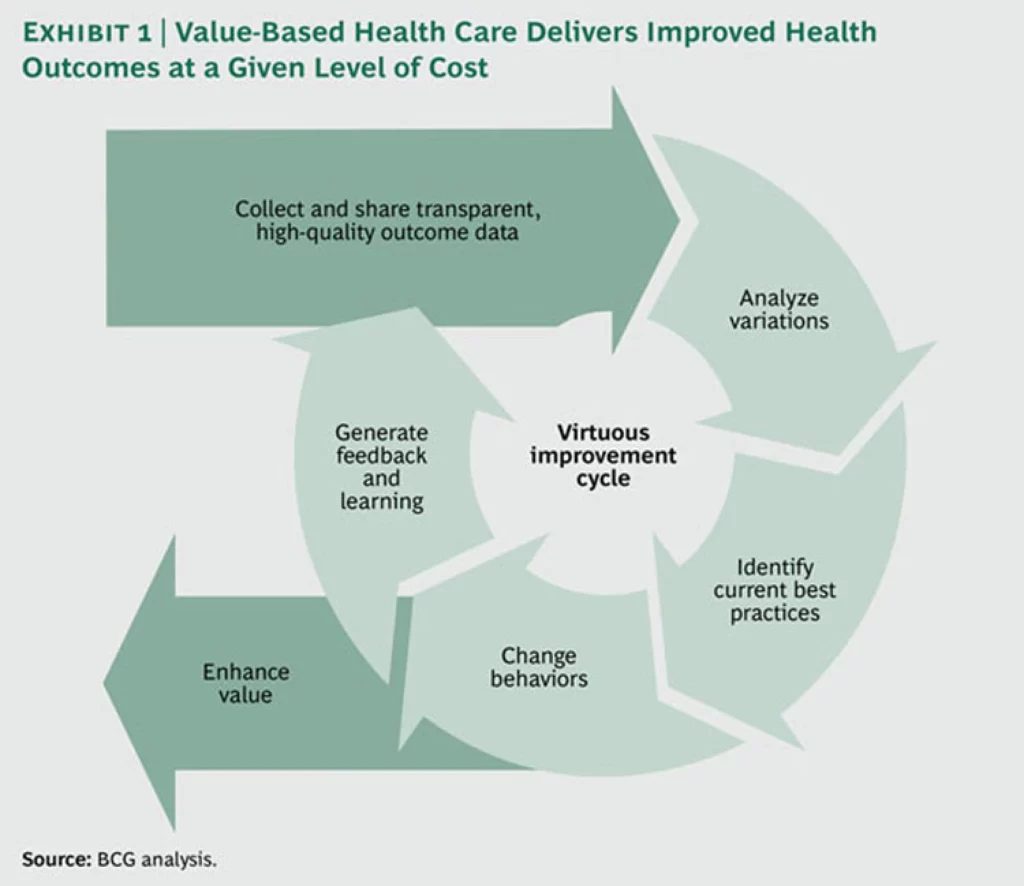
As a report by the Boston Consulting Group (BCG) notes: “Health systems around the world are systematically collecting, sharing, and analyzing health outcome data by disease group and population segment. By making this data standard and transparent, clinicians can benchmark and compare performance across care sites, document variations in health outcomes, identify best practices, and steer resources toward interventions and practices that have the highest value for patients.”
While oceans of this vital data are available, often only a trickle of useful information reaches the people who need it most. In addition, a good portion of the administrative costs in the healthcare system involve the collection, movement, and storage of data.
So why is data management so hard? There are three major factors:
- The number of parties involved – Everyone from the primary-care physician to the insurer to the pharmacy feels they “own the patient.” Yet none of them truly sees the whole picture.
- The multiplicity of data formats – Data is collected and stored in many different formats, such as FHIR, SOAP, HEDIS, and EDI 835/837. In addition, around 30 percent of healthcare information is unstructured data (such as doctors’ notes, X-rays and scanner images, audio/video files, and faxes).
- Silos of information – Each entity keeps its own records, but seldom are they shared efficiently.
Consider an everyday scenario that illustrates all three aspects of data management complexity.
- George, a 59-year-old male, comes to his doctor complaining of chest pains.
- The physician makes an initial assessment and is concerned enough that he refers him to a cardiologist.
- The cardiologist orders tests, diagnoses coronary occlusion, and recommends bypass surgery.
- The surgery is performed successfully, and George spends a week in a rehabilitation facility.
- New medications are added to his daily routine, and he is referred to providers for advice on exercise and improvements in his diet.
- George makes follow-up visits to his cardiologist at six-month intervals.
At every stage, there is an exchange of data among two or more of many stakeholders. Multiply this example of one patient with one condition, and you see the scale of the data-management challenge.
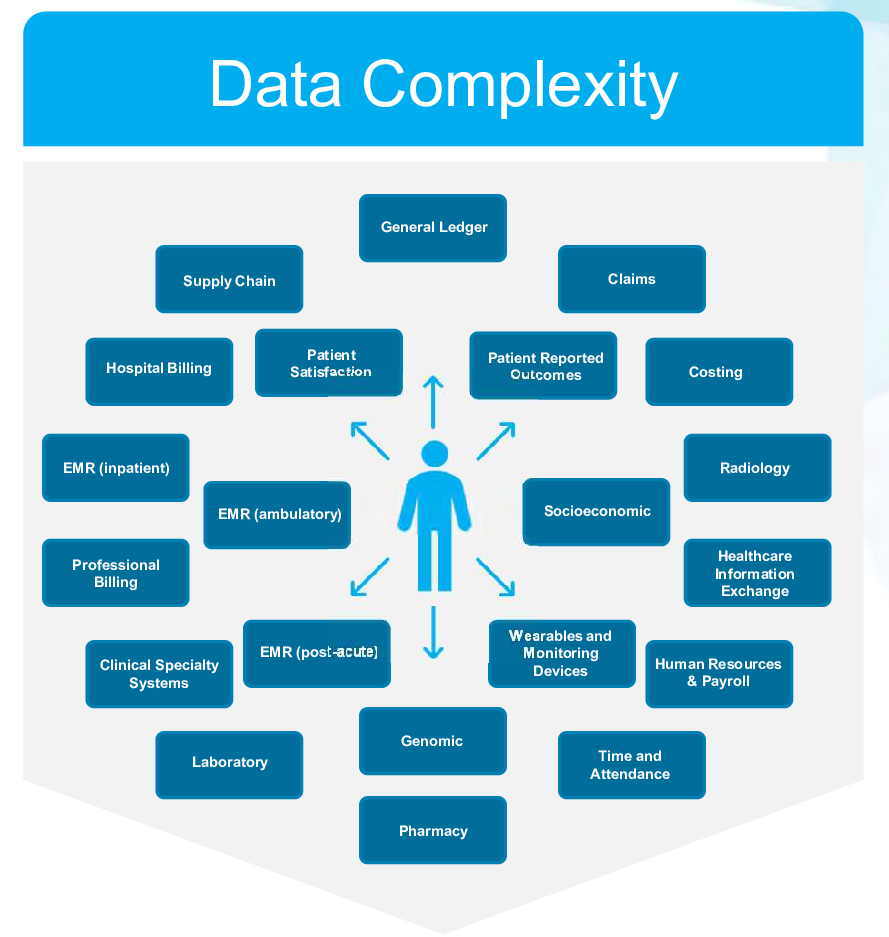
This graphic from Health Catalyst illustrates just how complex data management is in U.S. healthcare.
Here are some of the negative outcomes from information not being shared among all parties in a seamless and timely manner:
- Care for patients can be delayed, potentially leading to complications, incomplete diagnoses, and possible expensive emergency room visits.
- Providers may be unaware of relevant details about a patient’s case that are necessary to inform the correct treatment and care plan.
- Searches for required information can result in duplicate efforts, raising costs and adding delays.
- Current best-practices and innovations are not visible across stakeholders, which slows behavior change and evolution of treatment.
This chart from BCG shows how the VBC model can deliver better outcomes at a given level of cost.
Adoption of VBC principles also needs to go beyond large organizations – specifically, to smaller one- to five-person primary-care practices.
The Enormous Opportunities for Health Tech Innovators in VBC
For health tech entrepreneurs, the scale of challenges in VBC should be exciting rather than daunting. The potential for innovation and growth in VBC-related solutions is immense. For example, McKinsey estimates VBC may add $1 trillion in enterprise value by 2027, while Bain & Co. sees fee-for-value arrangements capturing 15-20 percent share from fee-for-service providers by 2030. In these early innings of the VBC transition, effectively tracking outcomes and reducing cost has become increasingly important with the CMS proposing greater scrutiny around Medicare Advantage risk adjustment.
There is tremendous opportunity for startups that contribute to integrated data records and workflow enablement across primary care, specialty, home care, and health systems. We see many examples of successful young and mature companies addressing this space, such as Lightbeam, Snowflake, Innovaccer, Closed Loop, Curitics Health, and AWS HealthLake just to name a few.
Many specialties have seen only minimal adoption of VBC to date (e.g., women’s health, cardiology, and behavioral health), leaving the field open to innovative providers. We also believe there is tremendous white space for underlying enablers who help these providers improve their data integration, risk-based contracting, patient engagement, and clinical workflows.
Norwest is focused on supporting entrepreneurs with innovative approaches to healthcare, as we have with current and past portfolio companies such as Clever Care, Diana Health, Kyo, Mindful Health Solutions, and Monogram Health. All Norwest investments emphasize our values of doing well by doing good and choosing long-term rewards over short-term gains, which ultimately yields the best results for everyone. Our team seeks to partner with companies that will have a lasting impact, shifting towards a value-based care model or enabling providers with this transition.
Contact Irem Rami, Suraj Shah or Sam Lesser if you have ideas for a business that can help spread the benefits of VBC.







